Hospital stays are a significant component of healthcare costs and often place a heavy burden on patients and healthcare systems alike. Prolonged or unnecessary hospitalizations can lead to higher expenses, patient discomfort, and increased risks of complications such as infections. Reducing the length of hospital stays is, therefore, a critical objective for improving the overall efficiency of healthcare delivery. One of the most promising ways to achieve this is by using Artificial Intelligence (AI) to enhance predictive care and preventive health strategies.
AI’s ability to analyze vast amounts of data, recognize patterns, and predict outcomes offers new opportunities to prevent avoidable hospitalizations and manage health conditions before they worsen.
The Cost of Prolonged Hospital Stays
Hospital stays are costly not only because of medical treatments but also due to the resources required for extended care, such as staffing, facility use, and medical supplies. In the U.S., hospital care accounts for about 31% of national healthcare spending, according to the Centers for Medicare & Medicaid Services (CMS). Prolonged hospital stays also increase the likelihood of hospital-acquired infections and other complications, further driving up healthcare costs.
For patients, long hospitalizations can lead to physical and emotional stress, as well as financial burdens from high medical bills and lost income from missed work. Reducing unnecessary hospital stays is, therefore, essential for improving patient outcomes and reducing overall healthcare costs.

How AI is Reducing Hospital Stays
AI has the potential to revolutionize healthcare by predicting which patients are at risk of hospitalization, detecting early signs of disease exacerbation, and enabling preventive interventions. Below are key ways in which AI is reducing hospital stays:
Predictive Analytics for Early Intervention
One of the most powerful uses of AI in healthcare is predictive analytics, which involves using machine learning algorithms to analyze patient data and predict future health events. By recognizing patterns in patient health records, AI can identify individuals who are at high risk of hospital admission or readmission.
For example, predictive algorithms can analyze electronic health records (EHRs), lab results, and vital signs to identify patients who may be at risk of complications such as heart failure, respiratory distress, or sepsis. Once high-risk patients are identified, healthcare providers can intervene earlier with targeted treatments or preventive measures, potentially avoiding the need for hospitalization altogether.
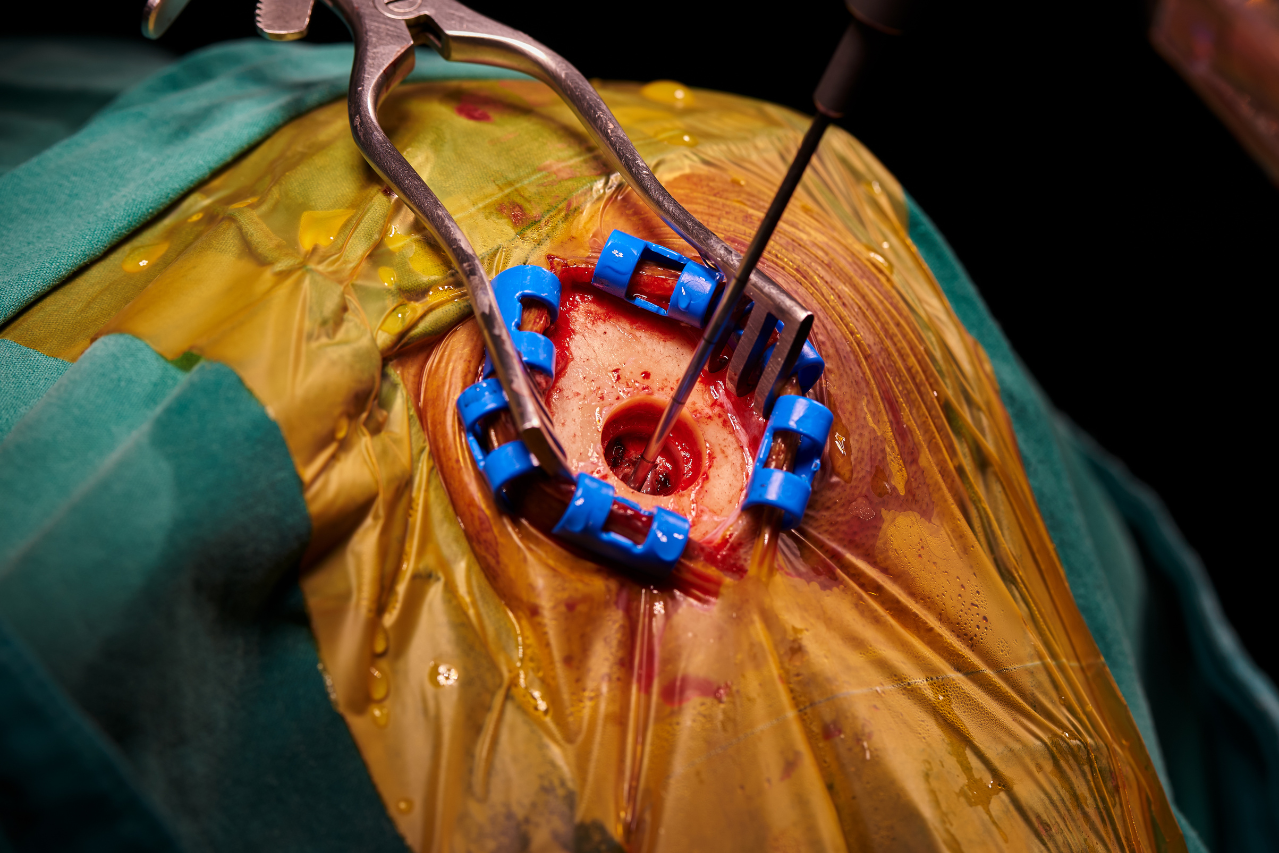
At Johns Hopkins Hospital, which developed the Sepsis Early Detection Tool. This AI tool monitors patients’ vital signs and lab results to predict the likelihood of sepsis, a life-threatening infection. Early detection allows clinicians to intervene promptly, significantly reducing the length of hospital stays for patients with sepsis.

Remote Patient Monitoring (RPM)
AI-powered remote patient monitoring (RPM) systems enable healthcare providers to track patients’ health in real-time, even when they are outside the hospital. These systems use wearable devices, sensors, and AI algorithms to continuously monitor patients’ vital signs, such as heart rate, blood pressure, and oxygen levels. If an abnormality is detected, the system can alert healthcare providers, enabling early intervention before the condition worsens.
For patients with chronic conditions like diabetes, heart disease, or COPD (chronic obstructive pulmonary disease), RPM can help prevent hospital admissions by identifying signs of disease exacerbation early. This reduces the need for emergency care or extended hospital stays, allowing patients to manage their conditions at home.
For example, Ochsner Health, a healthcare system based in Louisiana, has implemented an AI-driven RPM program for patients with chronic diseases. By monitoring patients’ vitals remotely, the program has successfully reduced hospital readmissions and kept patients out of the hospital.
AI-Powered Personalized Treatment Plans
Personalized medicine, enabled by AI, tailors treatment plans to individual patients based on their genetics, lifestyle, and medical history. AI algorithms can analyze vast amounts of patient data to predict how a patient will respond to a particular treatment, allowing healthcare providers to customize care plans that minimize hospital stays.
For example, in cancer care, AI systems like IBM Watson for Oncology are being used to recommend personalized treatment options based on the patient’s specific cancer type, genetic mutations, and clinical history. This level of precision in treatment planning can reduce the need for trial-and-error approaches, shortening the time a patient spends in the hospital and improving overall outcomes.
AI in Preventive Health
Preventive healthcare focuses on identifying and managing health issues before they require hospitalization. AI can analyze data from multiple sources, including EHRs, wearable devices, and social determinants of health, to predict which individuals are at risk for developing chronic conditions such as diabetes or hypertension. By intervening early, healthcare providers can help patients adopt lifestyle changes or take medications that prevent disease progression.
In the context of preventive care, AI can also be used for population health management, where healthcare providers use data analytics to identify trends and target high-risk populations for preventive interventions. For example, AI-driven tools can help predict flu outbreaks or identify areas with high rates of diabetes, allowing healthcare providers to deploy resources more effectively and reduce hospitalizations in those communities.
AI and Early Detection of Chronic Conditions
At Mount Sinai Health System in New York, researchers have developed an AI model known as Deep Patient, which can predict the likelihood of patients developing chronic conditions like liver disease or diabetes. Deep Patient uses deep learning algorithms to analyze vast amounts of patient data and identify patterns that are invisible to the human eye. By predicting chronic disease progression early, healthcare providers can intervene before hospitalization is necessary, significantly reducing the length of hospital stays for these patients.

Challenges and Ethical Considerations
While AI has the potential to revolutionize healthcare, there are several challenges and ethical considerations that must be addressed:
1. Data Privacy and Security
AI relies on vast amounts of patient data to make accurate predictions. However, this raises concerns about patient privacy and data security. Healthcare organizations must ensure that AI systems comply with data protection regulations such as HIPAA in the U.S. and GDPR in Europe. Robust cybersecurity measures must also be implemented to protect sensitive patient information from data breaches.
2. Bias in AI Algorithms
AI algorithms are only as good as the data they are trained on. If the data contains biases—such as racial, gender, or socioeconomic disparities—these biases may be reflected in the AI’s predictions. For example, an AI system trained on data from predominantly white populations may not accurately predict outcomes for minority populations. To ensure equitable care, healthcare providers must regularly audit AI systems for bias and ensure that diverse data is used in training the algorithms.
3. Adoption and Integration of AI into Healthcare Systems
While AI holds great promise, there are challenges in integrating AI systems into existing healthcare infrastructures. Many healthcare providers are still reliant on legacy systems that may not be compatible with advanced AI platforms. Additionally, healthcare staff need to be trained to use AI tools effectively, and there may be resistance to adopting new technologies.
To address these challenges, healthcare organizations must invest in AI infrastructure and provide adequate staff training to ensure a smooth transition.
AI’s role in predictive care and preventive health is paving the way for a future where hospital stays are significantly reduced. From early detection of diseases and personalized treatment plans to remote patient monitoring and population health management, AI is transforming the way healthcare is delivered.
By intervening early and preventing disease progression, AI not only improves patient outcomes but also reduces the financial burden on healthcare systems. However, to fully realize the potential of AI, healthcare providers must address challenges related to data privacy, bias, and integration into existing systems.
As AI continues to evolve, its ability to reduce hospital stays and improve patient care will only grow, offering a more efficient, cost-effective, and patient-centered healthcare system.
Sources:
- Centers for Medicare & Medicaid Services. (2021). National Health Expenditure Data.
- Johns Hopkins Hospital. AI Tools for Sepsis Early Detection.
- Mount Sinai Health System. AI in Chronic Disease Prediction: Deep Patient.
- Ochsner Health. AI-Powered Remote Patient Monitoring Program.
- IBM Watson for Oncology. AI in Personalized Cancer Treatment.