Diagnosing psychiatric conditions has traditionally relied on patient self-reports, clinical interviews, and standardized questionnaires. However, these methods are often subjective, and patients may not always accurately describe their symptoms. AI offers more objective tools for diagnosing mental health disorders by analyzing behavioral, biological, and environmental data.
AI in the Early Diagnosis of Depression: Depression is one of the most prevalent mental health conditions globally, yet it often goes undiagnosed or misdiagnosed. AI algorithms can help identify early signs of depression by analyzing language use, social media activity, and behavioral patterns. For example, researchers have developed AI tools that analyze the language used in social media posts, emails, and text messages to detect signs of depression. A study published in Nature demonstrated that AI could accurately predict the onset of depression by analyzing changes in a person’s language, such as the increased use of negative words or a shift in sentence structure, before the patient even seeks help .
AI-powered tools like Woebot, an AI-driven chatbot, interact with users via text and track patterns in their responses, identifying emotional and linguistic cues that indicate depression or anxiety. These tools use natural language processing (NLP) to analyze users’ responses and detect subtle changes in mood over time, providing early diagnosis and timely interventions .
AI in Schizophrenia Diagnosis: Schizophrenia is another psychiatric disorder where early diagnosis is crucial for improving long-term outcomes. AI can assist in identifying early signs of schizophrenia by analyzing speech patterns, facial expressions, and even genetic data. A study published in Schizophrenia Research demonstrated that AI algorithms could detect speech abnormalities, such as disorganized thinking and incoherent speech, which are often present in the early stages of schizophrenia. These tools can analyze subtle shifts in speech that human clinicians might miss, allowing for earlier detection and intervention .
Additionally, researchers are exploring the use of AI to analyze neuroimaging data to identify structural changes in the brain associated with schizophrenia. AI models trained on large datasets of brain scans can detect subtle differences in brain structure and function, providing an objective tool for diagnosing schizophrenia early in its progression.
AI and Autism Spectrum Disorder (ASD) Diagnosis: AI is also being used to aid in the diagnosis of autism spectrum disorder (ASD), a condition that affects communication and social interaction. Early diagnosis and intervention are crucial for improving outcomes in children with ASD. AI can analyze video recordings of children’s behaviors, such as facial expressions, eye movements, and social interactions, to identify signs of autism more quickly than traditional assessments.
One AI tool, Cognoa, has been FDA-approved for diagnosing autism in children as young as 18 months. Cognoa uses machine learning algorithms to analyze video recordings and parent-reported data to identify patterns indicative of autism. This early diagnosis allows for timely interventions, such as speech and behavioral therapies, that can improve a child’s long-term development.
Personalized Treatment Plans in Psychiatry
Once a mental health condition has been diagnosed, AI plays a crucial role in developing personalized treatment plans that account for individual patient differences, such as genetic predispositions, treatment history, and lifestyle factors. Personalized care in psychiatry is essential because mental health disorders often vary widely in their presentation and response to treatment. What works for one patient may not be effective for another.
AI in Personalized Medication Management for Depression: Managing depression often involves a trial-and-error process to find the right medication and dosage for each patient. AI is helping to streamline this process by analyzing data from genetic tests, patient histories, and real-time symptom tracking to recommend the most effective antidepressants for individual patients.
For example, AI-powered tools like the GeneSight test use pharmacogenomics—the study of how genes affect a person’s response to medications—to predict how patients will respond to different psychiatric medications. By analyzing a patient’s genetic profile, the GeneSight test provides personalized recommendations for which antidepressants or antipsychotics are most likely to be effective, reducing the time it takes to find the right treatment and minimizing side effects. A study published in The American Journal of Psychiatry found that patients who used AI-guided pharmacogenomic testing experienced significant improvements in their symptoms compared to those who followed traditional prescribing methods.
AI in Personalized Cognitive Behavioral Therapy (CBT): Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for anxiety, depression, and other mental health conditions. AI-powered virtual therapists are now offering personalized CBT sessions tailored to individual patients’ needs. Tools like Woebot and Wysa use AI to engage with users through text-based conversations, providing CBT techniques that are customized to the patient’s current emotional state. These virtual therapists use machine learning algorithms to analyze user responses and adjust their approach based on the patient’s progress .
In one study published in JMIR Mental Health, AI-powered CBT platforms were shown to be as effective as traditional, face-to-face therapy for reducing symptoms of anxiety and depression. By providing personalized interventions based on real-time data, these AI-driven tools make mental health care more accessible and adaptable to each patient’s unique needs.
AI and Personalized Treatment for Bipolar Disorder: Bipolar disorder is characterized by alternating episodes of mania and depression, making it particularly challenging to manage. AI can help psychiatrists personalize treatment by analyzing a patient’s mood patterns, medication responses, and lifestyle factors to predict mood swings and adjust treatment plans accordingly.
Mood-tracking apps like Moodfit and eMoods are powered by AI algorithms that analyze daily mood logs, sleep patterns, and medication adherence to predict when a patient is likely to experience a manic or depressive episode. This real-time data allows psychiatrists to adjust medications, recommend lifestyle changes, or schedule therapy sessions before the mood episode occurs, improving long-term outcomes for patients with bipolar disorder .
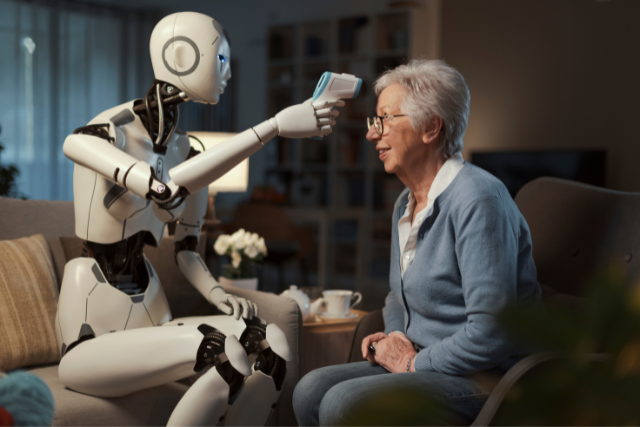
AI in Continuous Monitoring of Mental Health Conditions
Continuous monitoring is crucial for managing psychiatric conditions, especially those that require long-term care and medication management. AI-powered tools, including wearable devices and smartphone apps, are providing real-time monitoring of mental health patients, allowing for personalized and timely interventions.
AI and Wearable Devices for Mental Health Monitoring: Wearable devices, such as smartwatches and fitness trackers, are increasingly being integrated with AI to monitor physiological and behavioral indicators of mental health. These devices collect data on heart rate variability, sleep patterns, physical activity, and stress levels, which can then be analyzed by AI algorithms to detect early signs of mental health deterioration.
For example, Fitbit and Apple Watch have introduced features that track sleep and heart rate, which are critical indicators of mental health. AI algorithms analyze this data to detect patterns associated with mood disorders, such as increased heart rate variability during anxiety episodes or disrupted sleep patterns during depressive episodes. A study published in PLOS ONE found that AI-driven analysis of wearable data was able to predict depressive episodes with up to 80% accuracy, allowing for early intervention and personalized care adjustments.
AI-Powered Monitoring for Schizophrenia: Patients with schizophrenia often require continuous monitoring to manage symptoms and prevent relapses. AI-powered apps and wearables are helping to monitor patients’ mental states in real-time, providing insights into potential relapses before they occur. The app Mindstrong uses AI to analyze a patient’s smartphone usage patterns, such as typing speed, language use, and interaction frequency, to detect early signs of cognitive decline or psychotic episodes in patients with schizophrenia. By continuously monitoring these behavioral indicators, the app can alert clinicians to potential relapses, allowing for timely intervention and adjustments to the treatment plan .
AI and Suicide Prevention: AI is also being used to monitor patients at risk of suicide. By analyzing behavioral and physiological data, AI algorithms can identify individuals at risk and provide early warnings to clinicians. A study published in The American Journal of Psychiatry found that AI algorithms trained on patient data, including clinical records and social media activity, were able to predict suicidal behavior with greater accuracy than traditional risk assessments. AI tools such as Crisis Text Line use machine learning to analyze text messages sent by individuals in distress and prioritize those at highest risk of suicide for immediate intervention .
Challenges and Ethical Considerations
While AI has the potential to transform psychiatric care, several challenges and ethical concerns must be addressed. One of the primary challenges is ensuring the accuracy and reliability of AI algorithms, as errors in diagnosis or treatment recommendations could have serious consequences for patients. Additionally, there are concerns about data privacy, particularly when sensitive mental health information is involved. It is essential to ensure that AI tools comply with stringent data protection regulations, such as HIPAA in the United States, to protect patients’ privacy.
There is also the potential for bias in AI algorithms. If the data used to train AI models is not representative of diverse populations, the resulting algorithms may be less accurate for certain demographic groups. For example, AI tools developed using data from predominantly white, middle-class populations may not perform as well for minority or low-income patients, exacerbating existing health disparities.
Despite these challenges, AI holds significant promise for improving the diagnosis, treatment, and monitoring of psychiatric conditions, particularly as the technology continues to evolve and become more sophisticated.
AI is revolutionizing the field of psychiatry by enabling more personalized care at every stage of mental health management, from early diagnosis to treatment planning and continuous monitoring. Whether it’s diagnosing depression through language analysis, tailoring medication for bipolar disorder based on genetic data, or using AI-powered wearables to monitor mental health in real time, AI offers powerful tools for providing individualized care to mental health patients.
By leveraging AI’s ability to analyze vast amounts of data and detect patterns that human clinicians may miss, psychiatrists can make more informed decisions, leading to better outcomes for patients. As AI continues to advance, its role in psychiatry will only grow, offering new opportunities for personalized care and improved mental health outcomes for millions of people worldwide.
Sources:
- “AI and Language Analysis for Early Depression Diagnosis,” Nature, 2021.
- “AI in Schizophrenia Diagnosis: Speech and Brain Imaging,” Schizophrenia Research, 2022.
- “Cognoa: AI-Driven Autism Diagnosis,” Pediatrics, 2021.
- “GeneSight and AI in Personalized Psychiatry,” The American Journal of Psychiatry, 2020.
- “AI-Powered CBT Platforms and Mental Health Outcomes,” JMIR Mental Health, 2021.
- “AI and Wearables for Depression Prediction,” PLOS ONE, 2023.
- “Mindstrong: AI and Schizophrenia Monitoring,” Journal of Clinical Psychiatry, 2021.
- “AI in Suicide Prevention: Crisis Text Line,” The American Journal of Psychiatry, 2022.