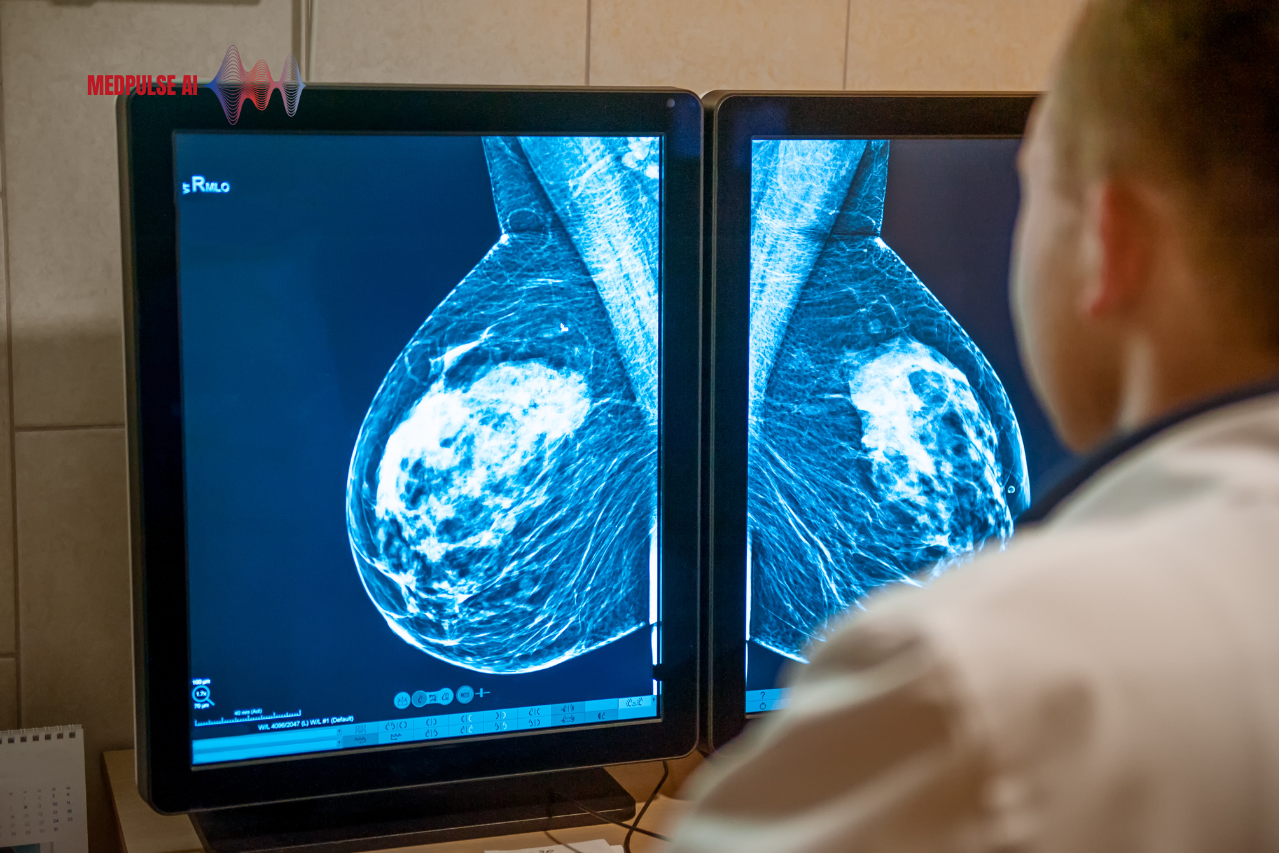
AdventHealth’s “GRACE” program, which stands for Genomics Risk Assessment for Cancer & Early Detection, is an innovative approach launched in August 2024 that combines genetics and artificial intelligence to assess early breast cancer risk. Currently operating at AdventHealth’s Waterford Lakes and Winter Park centers, the GRACE program enhances traditional mammogram screenings by integrating AI algorithms with patients’ family and personal medical histories. The AI-driven process refines risk analysis by examining thousands of anonymized cases, enhancing precision beyond conventional age-based assessments.
Why GRACE Is a Game Changer in Cancer Detection
Globally, breast cancer remains one of the most common cancers among women, and early detection can significantly increase survival rates.

The cancer prevalence data is based on approximate annual estimates cited by:
- Breast Cancer: Approximately 250,000 new cases annually (American Cancer Society).
- Lung Cancer: Around 116,000 new cases among women per year (National Cancer Institute).
- Colorectal Cancer: Roughly 64,000 new cases in women each year (American Cancer Society).
- Uterine Cancer: Estimated 62,000 new cases annually (American Cancer Society).
- Thyroid Cancer: About 56,000 new cases each year, with higher prevalence in women (National Cancer Institute).
- Ovarian Cancer: Approximately 21,000 new cases annually (American Cancer Society).
- Skin Cancer (Melanoma): Estimated 12,800 cases among women each year (American Cancer Society).
Traditionally, risk assessments have relied heavily on age and limited patient history, which can miss nuanced factors that contribute to individual risk. GRACE, however, employs AI algorithms that go beyond basic parameters, integrating a patient’s family and personal medical histories with data from thousands of anonymous patient records. This advanced AI-enhanced model includes image density analysis to assess breast density—a key risk factor that conventional screenings often overlook.

How AI Works Within the GRACE Program
The AI component of GRACE plays a dual role. First, it helps radiologists analyze imaging data by detecting subtle details in breast density that might escape the human eye. Second, embedded algorithms calculate a comprehensive risk score by considering an array of factors beyond just age. The program’s ability to continuously update a patient’s risk profile as new data is added—from genetic testing to imaging results—means that each patient receives a dynamic assessment that reflects their current health status.
By calculating a detailed risk score based on breast density, hormonal history, and genetic markers, GRACE provides a more individualized and accurate risk profile for each patient. As Dr. Wes Walker, AdventHealth’s Director of Genomics and Personalized Health, explains, “This program provides additional data to catch cancer early, or potentially prevent it in certain situations,” elevating breast cancer prevention to a new level.
Breast density is a measure of the relative amounts of fibrous, glandular, and fatty tissue in the breast, as seen on a mammogram. It’s significant because higher breast density can both mask tumors on mammograms and, independently, is associated with an increased risk of breast cancer. The American College of Radiology (ACR) classifies breast density into four categories:
- Category A: Almost Entirely Fatty
- This category means the breast is mostly composed of fatty tissue, with little fibrous or glandular tissue.
- Only about 10% of women fall into this category, which generally makes detecting abnormalities on a mammogram easier.
- Category B: Scattered Areas of Fibroglandular Density
- This classification indicates mostly fatty tissue with some scattered areas of denser fibrous and glandular tissue.
- Approximately 40% of women have this breast density, which presents a low to moderate risk for masking tumors.
- Category C: Heterogeneously Dense
- In this category, there is more fibroglandular tissue, making it moderately challenging to detect abnormalities.
- Roughly 40% of women are classified as heterogeneously dense, which can slightly increase the risk of breast cancer and makes mammogram interpretation more challenging.
- Category D: Extremely Dense
- This highest density category means the breast is mostly fibroglandular tissue, with very little fatty tissue, making mammogram readings difficult and increasing the risk of missed abnormalities.
- About 10% of women have extremely dense breasts, which are linked with a higher risk of breast cancer compared to the other categories.
For patients identified as high-risk, the program offers further steps, such as breast MRI scans or genetic testing, ensuring personalized, ongoing risk management. AI is employed both to analyze breast density and calculate individualized risk scores, factoring in detailed patient histories. AdventHealth’s integration of a Nurse Navigator to guide patients through their results further distinguishes the program, providing a human touch that supports patients in managing potential stress associated with high-risk results. The program aims to reach all 16 centers in Central Florida by 2025, targeting approximately 100,000 screenings per year.
The Role of the Nurse Navigator: High-Tech Meets High-Touch
A unique feature of the GRACE program is the inclusion of a dedicated Nurse Navigator. This professional supports patients by explaining test results, guiding them through the diagnostic process, and offering recommendations when high-risk factors are detected. Research has shown that patients facing high-risk diagnoses often feel overwhelmed, and having a support system to provide clarification and guidance makes a significant difference. This “high-tech meets high-touch” approach humanizes the experience, ensuring patients feel supported at each step of their healthcare journey.
Long-Term Impact and the Future of AI in Preventive Health
Once fully deployed across AdventHealth’s centers, the GRACE program is poised to make a substantial impact on breast cancer prevention in Central Florida. Early identification of high-risk individuals could lead to better outcomes, particularly as the program expands to other conditions where hereditary risks are a concern. This data-driven approach not only paves the way for more personalized healthcare but also aligns with a broader shift in healthcare towards proactive, preventive strategies.
AdventHealth’s approach exemplifies the potential of AI and genetics in preventive healthcare, offering a model for how such technology could improve early cancer detection and, ultimately, patient outcomes. This program represents a significant leap forward in personalized healthcare, especially for high-risk individuals who benefit from proactive care and continuous risk monitoring.
Are you interested in how AI is changing healthcare? Subscribe to our newsletter, “PulsePoint,” for updates, insights, and trends on AI innovations in healthcare.