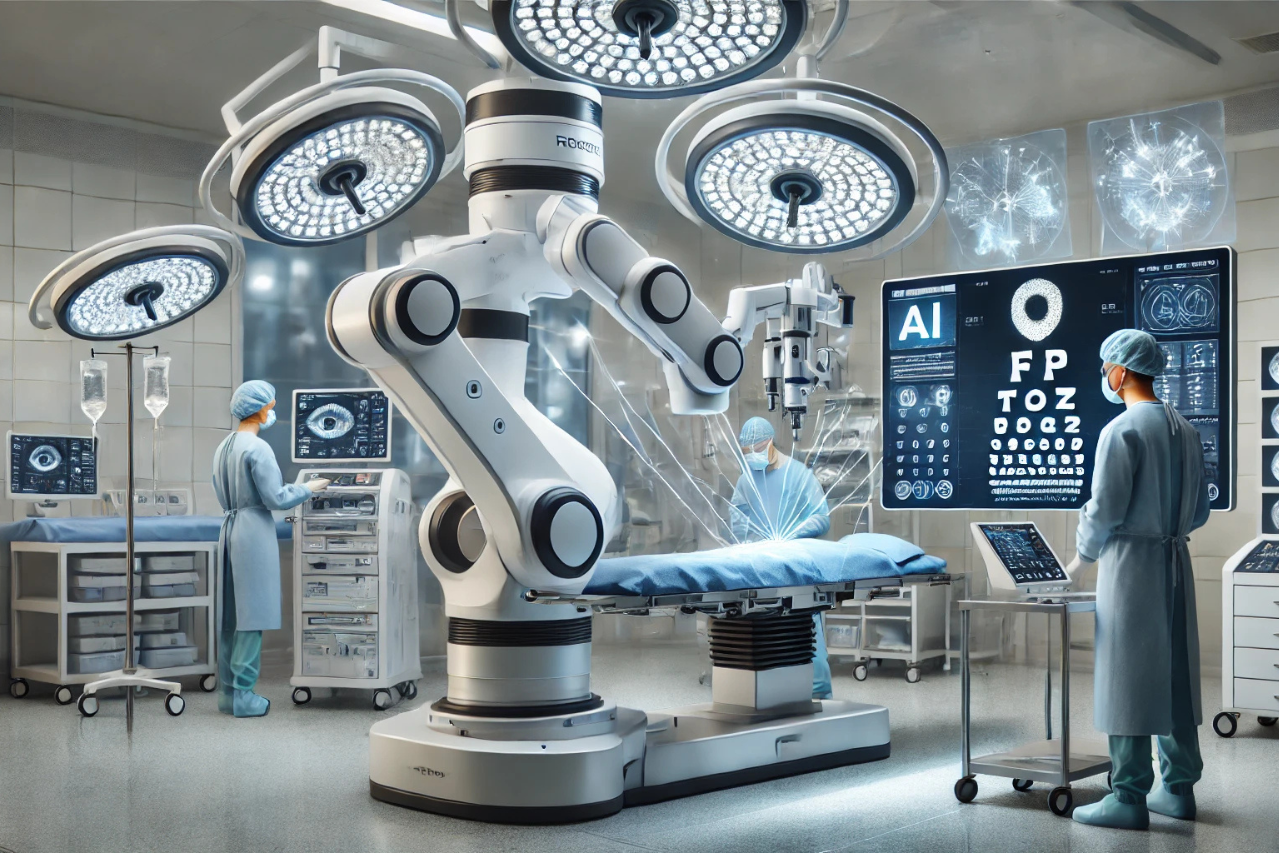
For the first time, a surgical robot has been trained to perform procedures by watching videos of experienced surgeons, marking a groundbreaking milestone in medical robotics. This innovation, led by researchers at Johns Hopkins University (JHU), demonstrates how imitation learning can be used to train robots to replicate complex human actions without requiring meticulous programming of every individual step.
The findings, presented at the prestigious Conference on Robot Learning in Munich, pave the way for true autonomy in robotic surgery, where robots could independently carry out intricate procedures.
Instead of programming robots to execute specific surgical moves, the researchers leveraged imitation learning. This method trains robots by showing them real-world examples of how tasks are performed. The team used the da Vinci Surgical System—a widely used robotic platform in operating rooms—to carry out three fundamental surgical tasks:
- Manipulating a needle.
- Lifting body tissue.
- Suturing.
The training model, combining imitation learning and machine learning architecture similar to what powers ChatGPT, transformed the visual input from surgery videos into robotic movements. While ChatGPT processes text, this AI model “speaks robot,” translating kinematics (robotic motion) into precise actions.
The system demonstrated remarkable adaptability, learning to perform these tasks as skillfully as human surgeons. Moreover, it showcased an ability to generalize its learning to unfamiliar surgical environments and even correct its own errors, such as retrieving a dropped needle without explicit programming.
The researchers trained the system using hundreds of videos recorded from wrist cameras mounted on da Vinci robots. These cameras captured surgeries performed by skilled surgeons across the globe, creating a rich dataset of real-world surgical expertise.
The da Vinci system, used in over 7,000 locations worldwide, generates a massive archive of videos for robots to “watch and learn.” However, the researchers noted that the system’s input data is inherently imprecise. To overcome this limitation, they designed the model to focus on relative movements rather than absolute, ensuring high accuracy despite noisy data.
Before this breakthrough, programming robots for even basic surgical tasks required hand-coding every action—a time-consuming and error-prone process. For example, modeling suturing for a single type of surgery could take years. The new system reduces this process to days, vastly accelerating the pathway toward fully autonomous surgical robots.
“This model learns in a couple of days what would have previously taken years of coding,” said senior author Axel Krieger, an assistant professor in JHU’s Department of Mechanical Engineering. “It’s a significant leap toward reducing medical errors and improving surgical outcomes.”
While the current study focused on discrete tasks, the researchers are now working to train robots for complete surgical procedures using imitation learning. This advancement could revolutionize healthcare by:
- Reducing surgeon fatigue: Robots could take over repetitive or time-intensive procedures, allowing surgeons to focus on complex decision-making.
- Improving accessibility: Autonomous surgical robots could provide high-quality care in remote or underserved regions where skilled surgeons are scarce.
- Minimizing errors: AI-driven precision may lead to fewer complications and better patient outcomes.
Moreover, as the model continues to learn, it could be adapted for various types of surgeries, from routine procedures to complex operations, making advanced robotic surgery more scalable and efficient.
As robotic surgery moves closer to full autonomy, the question of responsibility for medical errors becomes increasingly pressing. While these advanced systems promise precision, efficiency, and reduced human error, they also introduce complex ethical and legal challenges.
Who bears the accountability when something goes wrong—surgeons, manufacturers, hospitals, or AI developers? Unlike traditional surgeries where responsibility clearly falls on the human practitioner, autonomous robots blur these lines, creating a need for clear frameworks to address liability. As these technologies become more integrated into healthcare, establishing accountability is essential to ensure patient safety, build public trust, and foster responsible innovation in robotic-assisted medicine.
The Surgeon Overseeing the Procedure
Even with autonomous systems, most surgical robots today operate under the supervision of a human surgeon. This makes the surgeon the most likely party to be held accountable for errors. Their responsibilities include:
- Monitoring the robot’s actions.
- Intervening when necessary to correct potential mistakes.
- Ensuring the robot is set up and calibrated correctly before the procedure.
Challenges:
- If the robot operates autonomously beyond the surgeon’s direct control, how much responsibility falls on the surgeon? This gray area needs clear legal definitions.
The Manufacturer of the Robotic System
Robot manufacturers, such as those behind the da Vinci Surgical System, may share responsibility if errors occur due to:
- Hardware malfunctions: Mechanical failures, such as imprecise movements or tool breakage.
- Software bugs: Flaws in the robot’s programming or machine learning algorithms leading to incorrect decisions.
- Design flaws: If the system lacks safeguards or proper error-handling mechanisms.
Precedents: Product liability laws hold manufacturers responsible for defects in their products. If a robot’s failure can be traced back to the manufacturer, they could be liable for damages.
The Hospital or Healthcare Institution
Hospitals are responsible for ensuring the equipment they provide meets safety standards. Their liability could stem from:
- Improper training: If surgeons or staff are not adequately trained to use the robotic system.
- Maintenance lapses: Failing to regularly service and update the robot to ensure its proper functioning.
- Policy shortcomings: Allowing autonomous systems to operate without adequate oversight.
Challenges: Hospitals might argue that they relied on the manufacturer’s assurances about the robot’s safety, complicating accountability.
The AI Developers
If the error originates from the robot’s machine learning model, the responsibility could extend to the developers of the AI system. For instance:
- If the robot’s imitation learning misinterprets data from its training videos.
- If biases or gaps in the training dataset lead to incorrect actions.
Challenges: Developers might argue that their role ends with providing a functional model and that the responsibility lies with those implementing or deploying the system.
Regulatory Bodies and Standards Organizations
Regulatory agencies such as the FDA (in the U.S.) play a critical role in approving and monitoring robotic surgical systems. While they are not directly liable for errors, inadequate oversight could expose flaws in regulatory processes, such as:
- Insufficient testing protocols for autonomous capabilities.
- Failure to enforce clear guidelines for accountability in robotic surgeries.
Challenges: Regulators face the challenge of keeping up with rapidly evolving AI and robotic technologies, ensuring safety without stifling innovation.
Potential Resolutions and Emerging Models
- Shared Accountability Frameworks:
- Responsibility might be distributed among surgeons, manufacturers, and developers based on the root cause of the error.
- For example, if the error is mechanical, the manufacturer bears responsibility; if it’s user error, the surgeon or hospital may be at fault.
- Precedents from Autonomous Vehicles:
- Lessons can be drawn from how liability is handled for self-driving cars, where manufacturers often assume partial responsibility for accidents caused by their systems.
- Insurance and Risk Management:
- Hospitals and manufacturers may adopt robust insurance policies to cover liabilities arising from robotic surgeries.
- Some manufacturers may offer indemnity clauses to protect surgeons and institutions in case of errors.
- Transparent Error Logs:
- Robotic systems could include detailed error-logging mechanisms, making it easier to pinpoint responsibility in case of failures.
Ethical Implications
Accountability is not just a legal issue but also a matter of trust. Patients need clarity on:
- Who is ultimately responsible for their care?
- What safeguards are in place to prevent errors?
- How errors will be addressed, including compensation and corrective actions.
A clear legal and ethical framework will be essential to ensure that as robotic surgery becomes more autonomous, it remains safe, trustworthy, and equitable for all stakeholders.
Should Patients Know Who or What Will Perform Their Surgery?
Patient trust is a cornerstone of successful medical treatment, particularly when life-critical tasks are involved. As robotic systems take on more significant roles in surgery, the question of whether patients should know—and will know—who or what is performing their procedure is both ethical and practical.
Informed Consent: A Legal and Ethical Obligation
Transparency is a foundational principle of informed consent, which requires that patients be fully informed about the nature, risks, and benefits of their treatment before agreeing to it. This principle extends to robotic surgery, where patients should:
- Be explicitly told if a robotic system will perform their surgery or if a human surgeon will guide or assist the robot.
- Understand the role of the surgeon during the procedure—whether they will be actively controlling the robot, supervising its actions, or available only for emergencies.
- Receive details on the robot’s capabilities and limitations, including its track record and error rates.
Failing to provide this information could undermine patient trust and potentially result in legal repercussions for healthcare providers.
Patient Expectations in Practice
While most hospitals already disclose the use of robotic systems like the da Vinci Surgical System, the rise of autonomous robotics may lead to additional considerations:
- Clear Communication:
- Patients may want to know the extent of autonomy the robot will have. For instance, is the robot performing the entire procedure independently, or is a surgeon overseeing every step?
- Choice and Preferences:
- Some patients may prefer human-led procedures, citing concerns over the robot’s judgment in unexpected situations. Providing this choice can enhance trust and patient satisfaction.
Regulatory Requirements
Governments and medical boards may mandate disclosure about robotic involvement in surgeries as part of regulatory frameworks. Hospitals may also need to implement policies ensuring patients are fully aware of:
- The specific robotic system being used.
- The roles of both the robot and the surgical team during the procedure.
Technological Transparency
As AI-driven surgical robots gain autonomy, they could include features that make their performance more transparent:
- Pre-surgery briefings: Informing patients about how the robot works, including visualizations or simulations of the procedure.
- Post-surgery reports: Detailing the robot’s role and performance, including any deviations from expected actions.
Educating patients about the safety, reliability, and advantages of robotic surgery can help alleviate concerns. Providing accessible materials, such as videos, brochures, or interactive sessions, ensures that patients are not only aware but also comfortable with the technology.
Patients should—and likely will—be informed about who or what is performing their surgery. Providing this information is not only an ethical obligation but also essential for building trust in robotic systems. As these technologies evolve, the healthcare industry must prioritize transparency and communication to ensure patients feel confident and secure in their care.
The advancements achieved by the collaborative efforts of Johns Hopkins University and Stanford University mark a significant turning point in the field of robotic surgery. By harnessing the power of imitation learning, these researchers have demonstrated that surgical robots can be trained to perform complex procedures with the precision and skill of experienced human surgeons.
This breakthrough not only accelerates the path toward fully autonomous robotic systems but also holds the potential to redefine surgical practices worldwide—improving accuracy, reducing errors, and increasing access to high-quality care.
As this technology continues to evolve, it opens new possibilities for addressing surgeon shortages, enhancing patient outcomes, and democratizing advanced surgical techniques across diverse healthcare settings. However, it also introduces critical questions about safety, accountability, and patient trust that must be addressed with clear ethical and regulatory frameworks.
With ongoing interdisciplinary collaboration and a commitment to transparency, the integration of autonomous robotics into surgical practice could herald a future where innovation and humanity work hand in hand to transform global healthcare.