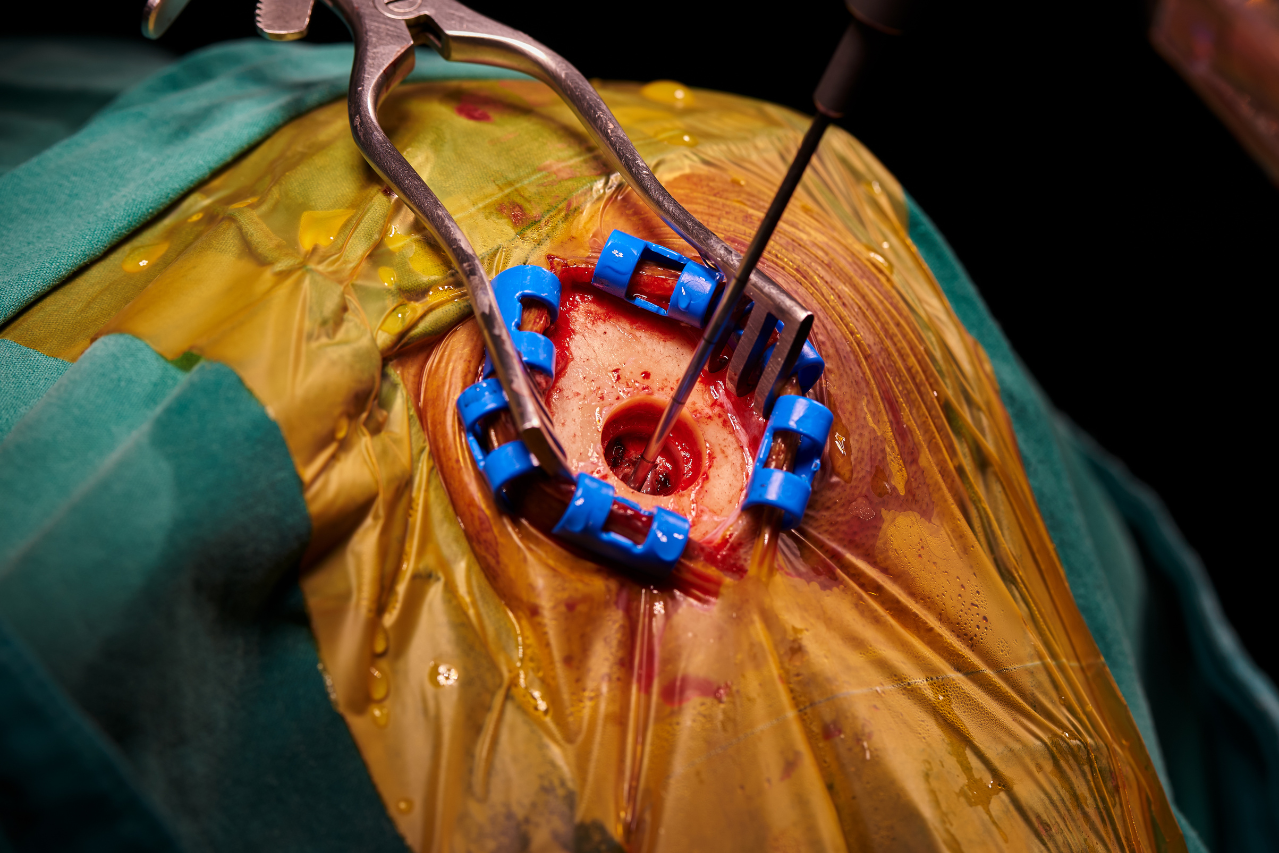
Surgical procedures, while often life-saving, come with inherent risks. Among these, alcohol consumption can complicate everything from anesthesia to wound healing, increasing the likelihood of infections, extended hospital stays, and other complications.
Despite the significant impact of alcohol on surgical outcomes, many patients who drink regularly do not receive a formal diagnosis of alcohol use disorder, which often leads to missed opportunities for preoperative intervention. This is where artificial intelligence (AI) is stepping in to make a difference.
Recent advancements in AI, particularly through natural language processing (NLP), are now being used to scan electronic health records (EHRs) for signs of risky alcohol consumption—signs that are often overlooked in traditional screening methods.
A new study by the University of Michigan has shown that AI can identify risky drinking behaviors in surgical patients by analyzing detailed notes within medical records, potentially saving lives and improving surgical outcomes.
Alcohol and Surgery: A Risky Combination
Research has long shown that alcohol consumption can significantly elevate the risks associated with surgery. Having more than a couple of drinks a day on average has been linked to a higher likelihood of infections, wound complications, pulmonary issues, and prolonged recovery times. Despite these risks, many patients may not be formally diagnosed with alcohol use disorders, leaving surgical teams unaware of the potential dangers.
In fact, many individuals who drink regularly don’t fall under the category of “alcohol use disorder” (AUD), which is typically the only diagnosis flagged in medical records. This leaves a large number of patients—those who consume alcohol at risky levels without a formal diagnosis—under the radar for surgical teams.
As Dr. V. G. Vinod Vydiswaran, lead author of the study, explains, “Given the excess surgical risk that can arise from even a moderate amount of daily alcohol use, and the challenges of implementing robust screening and treatment in the pre-op period, it’s vital that we explore other options for identifying patients who could most benefit from reducing use by themselves or with help, beyond those with a recorded diagnosis.”
AI in Action: Uncovering Hidden Risks
The study, published in Alcohol: Clinical and Experimental Research, utilized a form of AI known as natural language processing (NLP) to scan the medical records of surgical patients. By analyzing a patient’s entire medical history—beyond just the diagnosis codes—NLP tools are able to identify signs of risky drinking that might be recorded in notes from physicians or other healthcare providers.
These signs can include statements made in doctor’s notes about alcohol use or behavior patterns indicative of risky drinking, even if a formal diagnosis of alcohol use disorder is not present.
In the study, the researchers trained an AI model by allowing it to review 100 anonymous patient records from a surgical clinic. The AI then identified instances of risky drinking based on unstructured data within the records, such as doctor’s notes.
The results were compared to classifications made by expert human reviewers, and the AI model was able to identify risky drinkers with remarkable accuracy. According to the study, the AI matched the human expert classification 87% of the time. However, only 29% of those identified as risky drinkers had a diagnosis code related to alcohol in their medical records.
As Dr. Anne Fernandez, senior author and addiction psychologist at the University of Michigan’s Addiction Center, points out, “Surgical clinics that simply review the diagnosis codes listed in their incoming patients’ charts, and flag ones such as alcohol use disorder, alcohol dependence or alcohol-related liver conditions, would be missing many patients with elevated risk.”
AI’s Expanded Reach: Scanning Over 53,000 Records
The power of AI doesn’t stop at a small sample size. The researchers further tested the AI model by applying it to more than 53,000 anonymous patient records from the Michigan Genomics Initiative. The results were staggering.
The AI tool identified three times more patients with risky alcohol use than traditional methods based on diagnosis codes alone. While only 5% of patients were flagged using traditional codes, the AI flagged 15% of the patients for risky alcohol use.
This finding is particularly important because it demonstrates the potential of AI to capture a broader spectrum of patients who might otherwise go undiagnosed, allowing surgical teams to address alcohol-related risks proactively.
As Vydiswaran explains, “This evaluation of natural language processing to identify risky drinking in the records of surgical patients could lay the groundwork for efforts to identify other risks in primary care and beyond.”
Global Implications of AI in Preoperative Assessments
While this study was conducted at the University of Michigan, its implications are global. Many healthcare systems worldwide are beginning to explore the use of AI tools to enhance surgical safety by identifying at-risk behaviors like alcohol use.
- United Kingdom
In the UK, AI tools are being tested by the National Health Service (NHS) to improve patient screening, including detecting risky behaviors such as alcohol use. AI-powered systems could help doctors identify patients who are at risk for alcohol-related surgical complications, improving preoperative care and ultimately reducing recovery times and surgical costs. - Australia
Australia, known for its progressive approach to public health, is exploring AI in several healthcare settings, including surgical risk management. AI-powered tools are being used to detect alcohol-related risks in patients, particularly in rural or remote areas where healthcare providers may have limited time for comprehensive preoperative assessments. - Asia
Countries like Japan and South Korea are leveraging AI to better understand alcohol use and its impact on surgical risks. By customizing AI models to suit local cultural contexts, these nations are building sophisticated systems that can discreetly identify risky drinking behaviors, addressing a significant public health issue.
Cultural Sensitivity in AI Models
One of the challenges for AI adoption in healthcare is its ability to adapt to different cultural and demographic contexts. Alcohol consumption and its societal acceptance vary widely across cultures, which means that AI tools need to be flexible enough to account for regional differences in drinking behaviors.
In some countries, such as in parts of the Middle East where alcohol is stigmatized or banned, AI models must be sensitive to underreporting or misrepresentation of alcohol use. Conversely, in Western nations where moderate drinking is more socially accepted, AI models must be capable of distinguishing between safe drinking habits and those that put patients at risk.
AI’s ability to analyze unstructured medical notes and recognize subtle patterns is essential to ensuring accurate risk identification across diverse populations.
As Vydiswaran suggests, “Essentially, this is a way of highlighting for a provider what is already contained in the notes made by other providers, without them having to read the entire record.” This capability makes AI tools versatile and scalable for use in diverse healthcare systems globally, helping to improve patient outcomes no matter the region or culture.
Improving Patient Outcomes Through AI
The success of AI in identifying risky alcohol use during preoperative screenings is just the beginning. As AI tools continue to evolve, they have the potential to play a pivotal role in a range of healthcare settings.
By extending beyond the operating room, AI models could eventually be used to detect other lifestyle factors—such as smoking, obesity, and chronic disease—that impact patient outcomes. In primary care, AI could flag risk factors earlier, allowing for timely interventions that reduce the need for costly and complex medical treatments later on.
Furthermore, as AI technologies become more refined, they will be able to offer tailored recommendations for healthcare providers based on individual patient profiles, ensuring that interventions are not only effective but also personalized to each patient’s unique circumstances.
AI as a Game-Changer in Surgical Risk Management
The ability of AI to detect risky alcohol use in surgical patients is a significant breakthrough in healthcare. By scanning unstructured data in medical records, AI tools offer a way to identify risks that would otherwise be overlooked, allowing for proactive intervention and better surgical outcomes.
As AI technology continues to improve, it has the potential to revolutionize not just preoperative care but healthcare as a whole, paving the way for safer surgeries, faster recoveries, and more personalized treatment strategies.
The findings from the University of Michigan study are just one example of how AI is changing the face of medicine. With the potential for global application, this technology could become an essential tool in healthcare systems worldwide, helping to reduce complications, save lives, and ultimately improve the quality of patient care.
Read more from our vetted sources:
Are you interested in how AI is changing healthcare? Subscribe to our newsletter, “PulsePoint,” for updates, insights, and trends on AI innovations in healthcare.