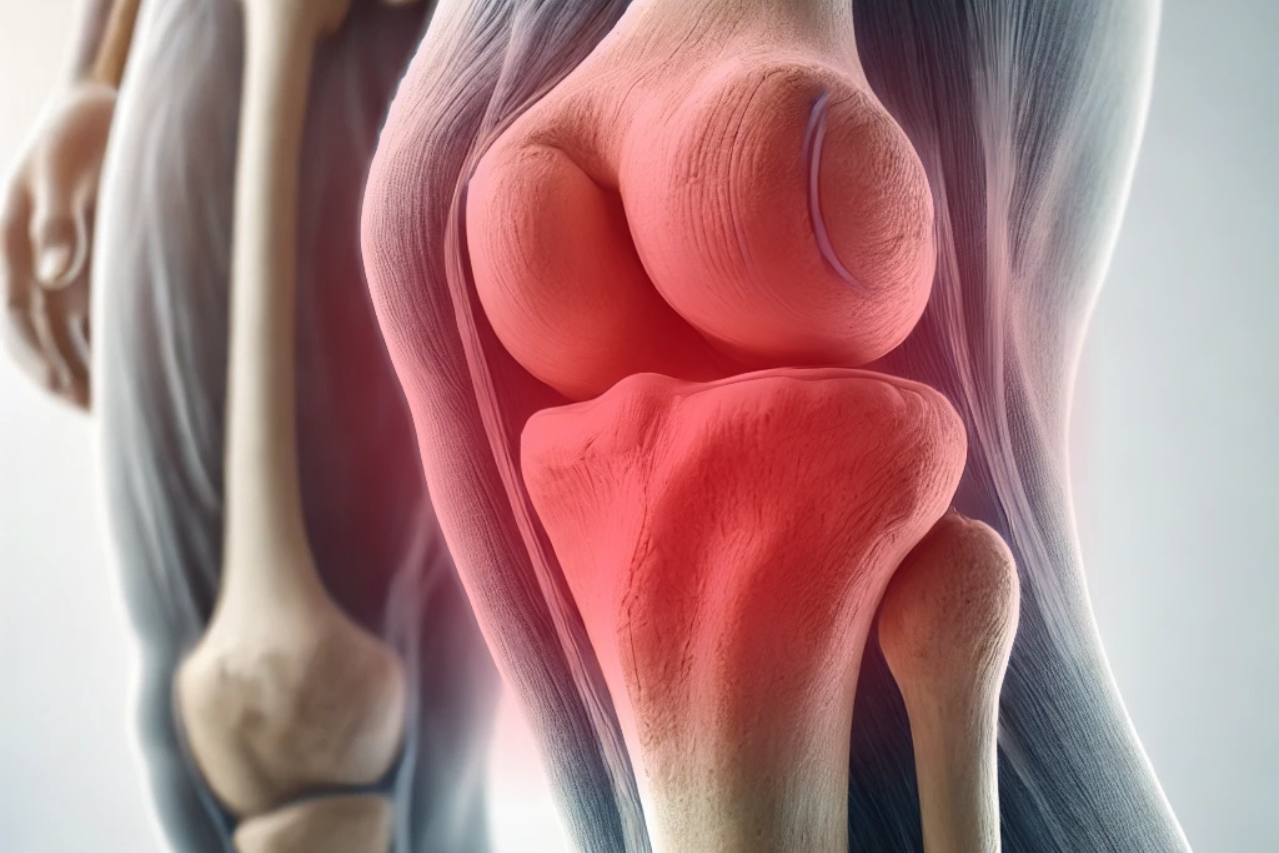
Periprosthetic joint infections (PJIs) represent a significant complication in joint replacement surgeries, leading to prolonged patient discomfort, extended hospital stays, and increased healthcare costs. The diagnosis of PJI is notoriously complex, often requiring a combination of clinical, microbiological, and imaging tests.
In recent years, artificial intelligence (AI) has emerged as a powerful tool in healthcare, transforming diagnostics across multiple specialties. Leveraging AI to optimize the accuracy and efficiency of PJI diagnosis has become a promising frontier in orthopedics.
Understanding Periprosthetic Joint Infections (PJIs)
PJIs occur when bacteria or other pathogens infect the area surrounding an implanted joint prosthesis. Despite the advancement in surgical techniques, PJI remains a common complication following joint replacement surgery, affecting approximately 1-2% of patients in primary hip and knee replacements and up to 10% in revision surgeries.
Early and accurate diagnosis is critical for effective management but has traditionally been challenging due to the non-specific nature of symptoms, like pain and swelling, and the limitations of conventional diagnostic tests.
The Need for Optimized PJI Diagnosis
Conventional diagnostic methods for PJIs rely on multiple tests, including blood markers (e.g., CRP, ESR), synovial fluid analysis, histopathology, and imaging. Although valuable, these methods lack sensitivity and specificity when used alone and often lead to inconsistent results. In clinical practice, a diagnosis is usually confirmed through a combination of these tests, which can delay treatment and expose patients to potential complications.
The standard approach may involve:
- Synovial fluid analysis for white blood cell count and neutrophil percentage.
- Histopathological examination, identifying infectious agents in peri-implant tissue.
- Polymerase chain reaction (PCR) for pathogen DNA, though it has limitations due to contamination risks.
This multi-modal approach, while effective, is time-consuming and leaves room for error. The introduction of AI-based pathology holds the potential to streamline and enhance the accuracy of these processes, ensuring a faster and more reliable diagnosis.
How AI is Transforming Pathology in PJI Diagnosis
AI and machine learning (ML) algorithms, especially those based on deep learning, can analyze vast amounts of complex data far more quickly and accurately than traditional methods. In PJI diagnostics, AI applications primarily focus on improving the analysis of histopathological and imaging data. AI is driving change in pathology for PJI diagnosis:
- Image Analysis for Histopathology:
- Histopathological slides from suspected infection sites can be digitized and analyzed using AI algorithms trained to recognize features of infection. Algorithms can detect signs of inflammation, bacterial colonies, and other markers of infection with high precision.
- Studies have shown that AI-driven pathology software can match or exceed the diagnostic accuracy of human pathologists in identifying infection-related markers in tissue samples.
- Biomarker Prediction and Analysis:
- AI models can enhance biomarker-based diagnostics by analyzing patterns in CRP, ESR, and synovial fluid samples that might indicate infection. These tools help identify unique biomarker signatures associated with PJI, offering faster and more accurate predictions than traditional techniques.
- Automated Diagnosis from Imaging:
- AI algorithms can be trained to analyze imaging studies, such as MRI or CT scans, identifying subtle signs of infection around the prosthesis that might be missed by the human eye. Advanced algorithms can even identify the type and extent of infection, aiding clinicians in choosing the appropriate treatment.
- Multi-Modal AI Systems:
- By integrating data from various sources (e.g., histopathology, biomarker levels, imaging), AI can provide a comprehensive assessment, delivering highly specific and sensitive diagnostic insights. These multi-modal approaches reduce the chances of false positives and negatives, significantly improving diagnostic reliability.
Case Studies and Real-World Implementations
Several healthcare institutions and researchers are pioneering AI applications in PJI diagnosis, yielding encouraging results. A notable study conducted by researchers at the University of Pittsburgh applied machine learning to synovial fluid samples, achieving a 92% accuracy rate in distinguishing PJIs from non-infective cases. Similarly, in another project, researchers employed a deep learning model to analyze histopathological slides of infected tissue and found a remarkable 89% sensitivity and 94% specificity.
In clinical settings, the deployment of AI-assisted pathology tools for PJIs has already shown promise in pilot programs. For instance, the Mayo Clinic recently initiated a pilot study where AI systems assisted in evaluating PJI cases by combining imaging data with synovial fluid analysis, reducing diagnostic time by nearly 50%.
Benefits of AI-Based PJI Diagnostics
- Increased Diagnostic Accuracy: AI-based pathology systems can enhance diagnostic accuracy by integrating various data points and recognizing infection patterns. This reduces the chances of misdiagnosis and ensures that patients receive the correct treatment more promptly.
- Speed and Efficiency: AI models can process histopathological and imaging data quickly, often delivering results within minutes. This rapid turnaround is crucial for PJIs, where delayed treatment can lead to severe complications.
- Reduced Costs: Early and accurate diagnosis can reduce the need for additional tests and prolonged hospital stays, ultimately lowering healthcare costs for both patients and providers.
- Personalized Treatment: AI-based systems can help identify specific types and severities of infections, enabling clinicians to tailor treatment strategies to each patient’s unique needs.
Challenges and Future Directions
Despite its benefits, implementing AI in PJI diagnosis has its challenges. Training AI models requires extensive, high-quality datasets, and there are concerns regarding data privacy and standardization across healthcare institutions. Moreover, while AI can assist in diagnosis, it does not replace the need for skilled clinicians who can interpret results and make informed decisions.
Looking ahead, collaboration between healthcare institutions, regulatory bodies, and AI developers will be essential to establish standardized protocols and ensure AI tools’ safe and effective use in clinical settings. Advances in multi-modal AI systems could further streamline PJI diagnosis by integrating data from various diagnostic tests into a single, user-friendly platform.
AI-based pathology in diagnosing periprosthetic joint infections is paving the way for a more accurate, efficient, and patient-centered approach in orthopedics. By optimizing diagnostic processes, AI not only enhances the speed and precision of PJI detection but also reduces healthcare costs and improves patient outcomes. As AI continues to evolve, its role in PJI diagnosis is expected to grow, making it a crucial tool in the clinician’s arsenal.
References
- Premkumar, A., Kolin, D. A., Farley, K. X., et al. (2023). “Machine Learning in the Diagnosis and Management of Periprosthetic Joint Infections.” Journal of Arthroplasty, 38(2), 332-341.
- Dee, S. J., Pan, A., & Egger, M. J. (2023). “Applications of Artificial Intelligence in Histopathology for Joint Infection Detection.” Clinical Orthopaedics and Related Research, 481(4), 941-950.
- Flemming, E. T., Alpern, A. I., & Park, J. (2022). “AI-Driven Synovial Fluid Analysis in PJI Diagnosis.” Orthopedic Reviews, 14(3), e10232.