The rise of drug-resistant “superbugs” over recent decades signals a potentially dire future where antibiotics may no longer shield us from deadly pathogens, posing a grave threat to modern medicine—surgeries, cancer treatments, and even minor injuries could become perilous without reliable antibiotics. The solution demands urgent innovation in antibiotic discovery, manufacturing, and distribution—a complex task facing formidable economic and scientific obstacles. However, with the advancement of AI, we now have a powerful ally in addressing antimicrobial resistance (AMR).
Generative AI, with support from sound public policies, could significantly accelerate antibiotic discovery, addressing this global health crisis. Yet, achieving this requires cooperation across sectors: innovators, academic researchers, and government entities must work together to ensure breakthroughs move from the lab to the market. It’s a united effort that, when strategically coordinated, could leverage AI’s promise into real-world outcomes, keeping AMR at bay.
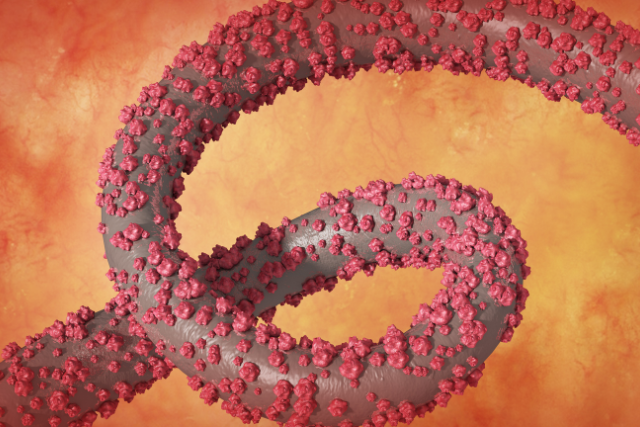
The Impending AMR Crisis
Antimicrobial resistance (AMR) is a rapidly escalating threat. According to The Lancet, by 2050, AMR could be responsible for close to 40 million deaths and contribute to 170 million more globally. This trend threatens the safety of a range of medical procedures, from hip replacements to C-sections. Without effective antibiotics, even minor infections could turn deadly. In the United States alone, more than 2.8 million drug-resistant infections occur annually, and recent CDC data indicates that hospital-acquired infections from seven resistant pathogens increased by 20% during the COVID-19 pandemic.

Unfortunately, creating a new generation of antibiotics has been hampered by a fractured economic landscape, where pharmaceutical companies struggle to offset the high costs of antibiotic development. Without a strong incentive structure, many companies find it financially unfeasible to bring new antibiotics to market.
The Economic ‘Valley of Death’ in Drug Development
Drug developers often speak of the “valley of death,” a term describing when scientific discoveries in the lab fail to reach human clinical trials, typically due to funding shortages. Antibiotics face an additional “second valley of death” even after FDA approval, given unique market challenges. Unlike treatments for chronic conditions, antibiotics are designed for short-term use, limiting their revenue potential. Additionally, new antibiotics often compete with cheaper, older alternatives, making it difficult to recover development costs. This economic mismatch has driven many companies, even those with FDA-approved antibiotics, to bankruptcy.
That is where AI comes in, offering a powerful tool to analyze vast datasets, identify new drug candidates, and predict resistance patterns, all of which help develop targeted, effective antibiotics faster and more efficiently than traditional methods allow.
Here’s how it works:
Data Collection and Preparation
- Initial Compound Screening: Researchers first screen thousands of chemical compounds to identify any that might have antibacterial properties. This involves testing different molecules on specific pathogens to see which compounds are effective in killing or inhibiting them.
- Data Generation: Results from this testing phase generate critical data on how each compound interacts with the bacteria. This data includes both successful and unsuccessful compounds, which provides AI with a broad range of patterns to learn from.
Training the Generative AI Model
- Pattern Recognition: The data collected is fed into a generative AI model, often leveraging machine learning techniques like deep learning. Artificial Intelligence analyzes the data to recognize patterns and relationships between the chemical structures and their antibacterial effects.
- Feature Extraction: The AI model identifies specific molecular features or configurations that are commonly present in compounds that successfully kill bacteria. This process teaches the AI model which structural characteristics are critical for antibacterial activity.
Generating New Molecules (In Silico)
- Molecule Design: With its learned patterns, the AI model can generate new molecular structures. Instead of just analyzing existing compounds, generative AI creates novel ones that have never been tested but are likely to possess antibacterial properties.
- Virtual Testing: The AI conducts simulations to predict how each new compound might interact with a particular pathogen. This allows researchers to evaluate the potential effectiveness of these compounds without physically synthesizing them, saving time and resources.
Filtering for Drug-Like Properties
- Toxicity and Absorption Prediction: After generating a pool of promising compounds, the AI model further evaluates them to identify any potential issues, such as toxicity or poor absorption. Filtering out compounds with undesirable properties helps ensure that only viable candidates move forward.
- Optimization for Safety and Efficacy: The AI model can also help fine-tune these new molecules to enhance their safety profile, ensuring they have minimal side effects while maximizing their antibacterial power.
Lab Validation and Testing
- In Vitro Testing: The top compounds identified by the AI undergo laboratory testing to confirm their antibacterial effectiveness. Researchers grow bacteria in petri dishes and test the AI-generated compounds to verify their real-world effects.
- In Vivo Testing: If a compound shows promise in the lab, it progresses to testing in living organisms to evaluate its safety and efficacy in complex biological systems.
Clinical Trials and Approval Process
- Clinical Trials: Compounds that prove successful in lab tests enter the traditional clinical trial process, starting with Phase I trials to assess safety in humans. Each successive phase evaluates the compound’s effectiveness, side effects, and optimal dosage.
- FDA Approval and Market Release: Once a compound successfully passes all clinical trial phases, it seeks approval from regulatory bodies, like the FDA, to be manufactured and distributed as a new antibiotic.
Benefits of Using AI in Antibiotic Discovery
- Time and Cost Savings: AI significantly reduces the time and costs associated with the discovery phase, often cutting years from the typical drug development cycle.
- Higher Success Rates: By focusing only on the most promising compounds, AI improves the likelihood of success, as researchers can prioritize the most viable candidates.
- Adaptability: As pathogens evolve, AI can quickly adapt and generate new compounds in response, which is crucial in the fight against rapidly mutating superbugs.
By compressing timelines and focusing efforts on the most promising compounds, AI is revolutionizing how antibiotics are discovered, giving researchers a strategic advantage in addressing antimicrobial resistance (AMR). This AI-enabled process opens up new possibilities for discovering treatments that might otherwise take decades to develop through traditional methods.
AI as a Game-Changer in Antibiotic Discovery
Artificial Intelligence offers a promising solution. Pharmaceutical leaders like Pfizer, AstraZeneca, and Janssen already use predictive AI to streamline various stages of drug development, from identifying chemical candidates to analyzing clinical trial data. Generative AI goes a step further by creating new molecular structures that could serve as the building blocks for antibiotics. This novel capability is already accelerating antibiotic research, saving companies valuable time and resources. For example, early estimates suggest that generative AI could reduce the drug development timeframe from 4.5 years to just 2.5 years, with costs potentially decreasing by two-thirds.
One company pioneering this approach is collaborating with the Massachusetts Institute of Technology’s Collins Lab. Their generative AI platform analyzes chemical properties of compounds that target pathogens, generating new structures for further testing. This method provides an efficient and scalable approach to antibiotic discovery, bringing us closer to a future where AI-designed antimicrobials are readily available.

Public Policy: An Essential Companion to AI-Driven Innovation
While AI-driven discovery represents a significant leap, bridging the second valley of death requires additional support. This is where public policy steps in. In the United States, the proposed PASTEUR Act aims to support antibiotic developers through a subscription-style payment model, allowing companies to receive consistent revenue independent of sales volume. This system would enable the government to provide access to new antibiotics for federal healthcare programs, ensuring these drugs are available when needed.
The UK has implemented a similar model, recently approving two candidate antibiotics under a subscription program. Japan and Canada are also considering comparable approaches. By reducing market dependence on sales volume, these policies create a more sustainable environment for antibiotic innovation.
The Future of AMR Management with AI
Generative AI has potential beyond antibiotic discovery. Its applications extend to personalized treatment recommendations, vaccine development, cancer diagnostics, and more. As we advance in this field, the combined efforts of innovative AI technology, robust public policy, and global collaboration can give us a much-needed advantage in the fight against superbugs. But these initiatives must start now—before resistance levels reach critical thresholds. Only by acting decisively can we harness AI’s capabilities to protect the future of medicine and keep AMR in check.
Are you interested in how AI is changing healthcare? Subscribe to our newsletter, “PulsePoint,” for updates, insights, and trends on AI innovations in healthcare.